Funding shortages undermine continuity of mobile health clinics in vulnerable West Bank communities
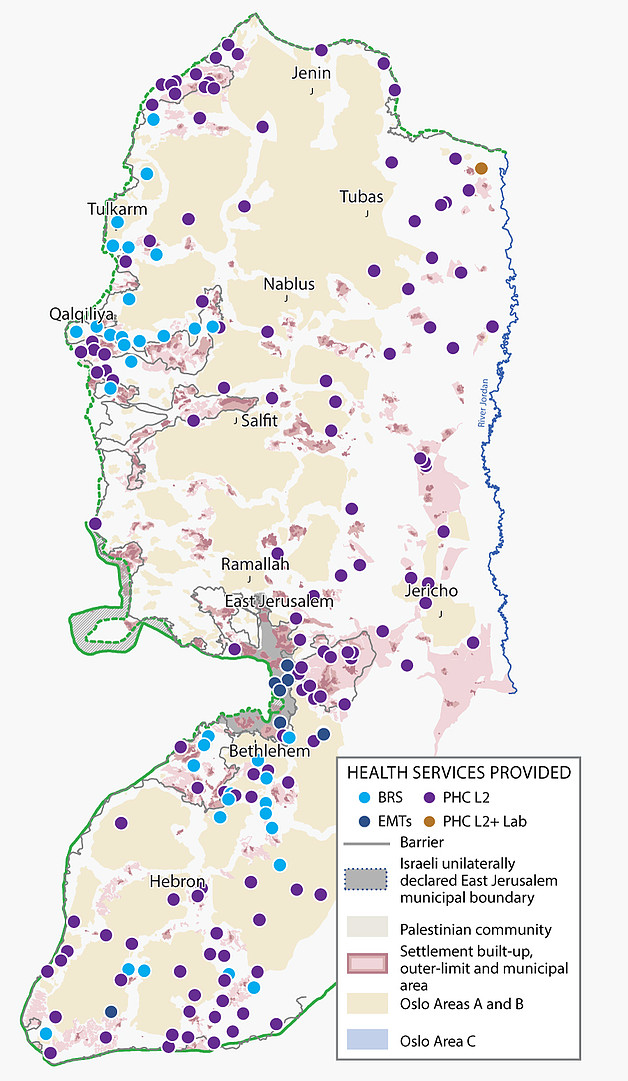
 Over 220,000 Palestinians living in 189 communities across the West Bank lack a permanent clinic and face critical challenges in accessing basic health services. These communities include, primarily, those located in Area C, in the Israeli-controlled parts of Hebron city (H2), and in the closed areas behind the Barrier (the Seam Zone). In many of these areas, the journey to the nearest clinic has lengthened because of the need to travel circuitous ways around settlements and barriers. Access to healthcare can be hampered by the unavailability or high costs of transportation, and in some communities, access to emergency services is challenging as even ambulances face delays.
Over 220,000 Palestinians living in 189 communities across the West Bank lack a permanent clinic and face critical challenges in accessing basic health services. These communities include, primarily, those located in Area C, in the Israeli-controlled parts of Hebron city (H2), and in the closed areas behind the Barrier (the Seam Zone). In many of these areas, the journey to the nearest clinic has lengthened because of the need to travel circuitous ways around settlements and barriers. Access to healthcare can be hampered by the unavailability or high costs of transportation, and in some communities, access to emergency services is challenging as even ambulances face delays.
The most vulnerable in these communities include women during pregnancy and childbirth; sick children and infants; the elderly; and the chronically ill or disabled. The knowledge that health access may be difficult and risky also acts as a psychological stressor that can directly affect health.
To mitigate this situation, ten organizations in the Health Cluster have been operating mobile clinics in vulnerable communities for the past few years.[1] A mobile health clinic team commonly includes a doctor, a nurse and a midwife who visit each community at least once a week. The clinics often operate in structures not intended for this purpose but provide primary health care services, curative treatment and some laboratory tests.
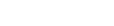
Communities served by mobile health clinics
Severe funding shortages since the beginning of 2018 have halted the work of these clinics serving nearly 13,000 people in 35 of the 189 communities. Unless additional funding is found immediately, mobile clinics serving another 11 communities in the Hebron area with a population of over 9,500 will also have to cease work.
On 20 February, the Humanitarian Fund for the OPT, managed by OCHA on behalf of the Humanitarian Coordinator, released $612,000 to UNRWA to guarantee the continued operation of six medical teams serving 39 communities, mainly in Area C, until mid-2018.[2] To secure the resumption and continuation of the mobile clinic service in all of the 189 communities through the end of 2018, additional $900,000 are required. While the Palestinian Ministry of Health is willing to cover the current and expected gaps, their capacity is estimated to be limited and insufficient.
The mobile clinic in Khan al Ahmar
The only health service available since the beginning of 2018 in a cluster of five Palestinian Bedouin communities in the Jerusalem governorate known as Khan al Ahmar, is a mobile clinic run by the Palestinian Medical Relief Society (PMRS). Access by Khan al Ahmar’s residents to health facilities in East Jerusalem is restricted by the Barrier and the permit system, and the nearest permanent clinic is in Jericho, 20 kilometres away. Transportation costs to Jericho are often prohibitive for already impoverished families. Both residents and ambulance/health personnel servicing the community often report delays on the roads at flying checkpoints deployed by Israeli forces.

Nurse Nabila Mousa visits six Bedouin communities to the east of Jerusalem, including in Khan al Ahmar, every week:
“I am one of a small team of four comprising a general practitioner, two nurses and a midwife, who visit Khan al Ahmar every Wednesday. We operate in the local mosque, where we treat both acute and chronically ill patients. We also provide preventive care and health education, especially for women, including awareness raising on breastfeeding, pregnancy follow-ups, and early stage breast cancer screening. We also provide limited pharmaceutical services with a range of medications, including antibiotics and drugs for chronic and skin diseases, as well as oral contraceptives and condoms. On average, we treat 50-70 patients per week, 86 per cent of whom are women and children. We rely on solar energy to run the basic medical equipment.”
“We feel responsible for the lives of the people residing in these communities. We often get calls from our patients if we are ten minutes late and they keep asking us to come more frequently. In November 2011, due to funding shortages, PMRC had to halt the mobile clinic service in this area for six months and that was disastrous. Some patients with chronic diseases stopped taking their medication and their condition deteriorated. We also detected many cases of children suffering from extreme skin and respiratory conditions that would have been easily treated if our services had not stopped. At that moment, I realized the critical importance of our work.”
Khan al Ahmar communities, inhabited by about 100 families, are located next to an area planned by the Israeli authorities for the expansion of the Ma’ale Adummim settlement (the E1 plan). They are among the 46 Palestinian Bedouin communities in the central West Bank at risk of forcible displacement due to the coercive environment generated by Israeli practices, including pressure to relocate the community.[3] A hearing at the Israel Supreme Court, on a petition against the demolition of the largest of the five Khan al Ahmar communities (Abu al Helu) is expected by the end of April.
* This article was contributed by the Health Cluster.
[1] The organizations are: HI: Humanity & Inclusion; UNRWA: The United Nations Relief and Works Agency; Dis-Vi: Italian NGO; CARE International; PMRS: Palestinian Medical Relief Society; MoH: Ministry of Health; HWC: Health Work Committees; MEDICO International; MAP-UK: Medical Aid for Palestinians; and PRCS: Palestine Red Crescent Society.
[2] An additional $288,000 were allocated by the HF to UNRWA to maintain food distribution to Bedouin and herding communities in Area C for a period of six months. See Statement by the Acting Humanitarian Coordinator.
[3] The findings of a needs assessment carried out by OCHA in 2017 among the 46 affected communities is available on an interactive database.